Chorioangioma
Case Study Posted By : Dr. TLN Praveen

Description
Case Presentation
- 22-year-old primigravida was referred to our institute for an anomaly scan.
- There was history of consanguinity.
- She was normotensive with normal GTT.
- Her blood parameters were normal with normal hemoglobin of 12gms/dl.
- Fundal height was corresponding to period of gestation.
- She was perceiving good fetal movements.
Ultrasound Features
- Ultrasound examination revealed a single live intrauterine gestation in cephalic presentation.
- Fetal biometry and growth factors were corresponding to period of gestation
- Fetal biometry and the ultrasound assigned gestational age was corresponding to 22 weeks
- First trimester screening done elsewhere showed low risk for aneuploidies (1 in 3879 for T21).
- Fetal anomaly scan showed normal anatomy.
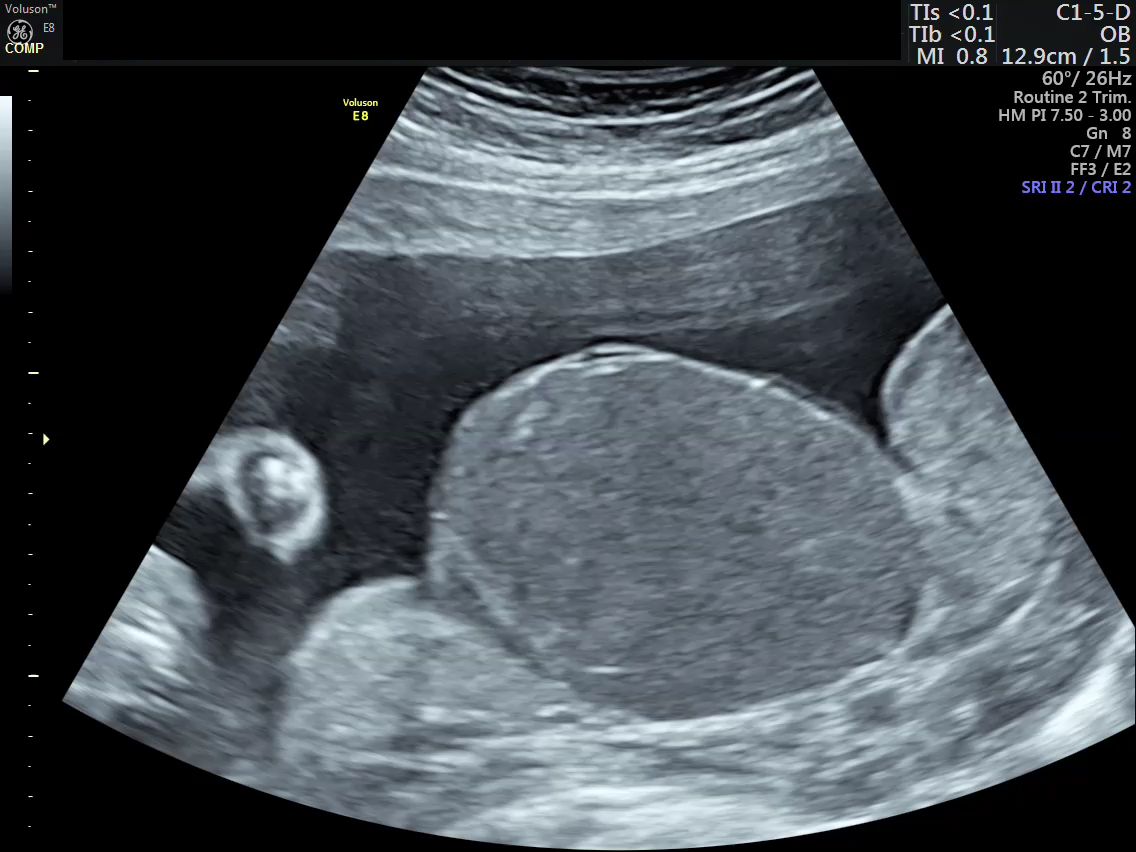
- The AFI (Amniotic fluid index) was 28 - suggesting mild hydramnios.( SVP 9 cms)
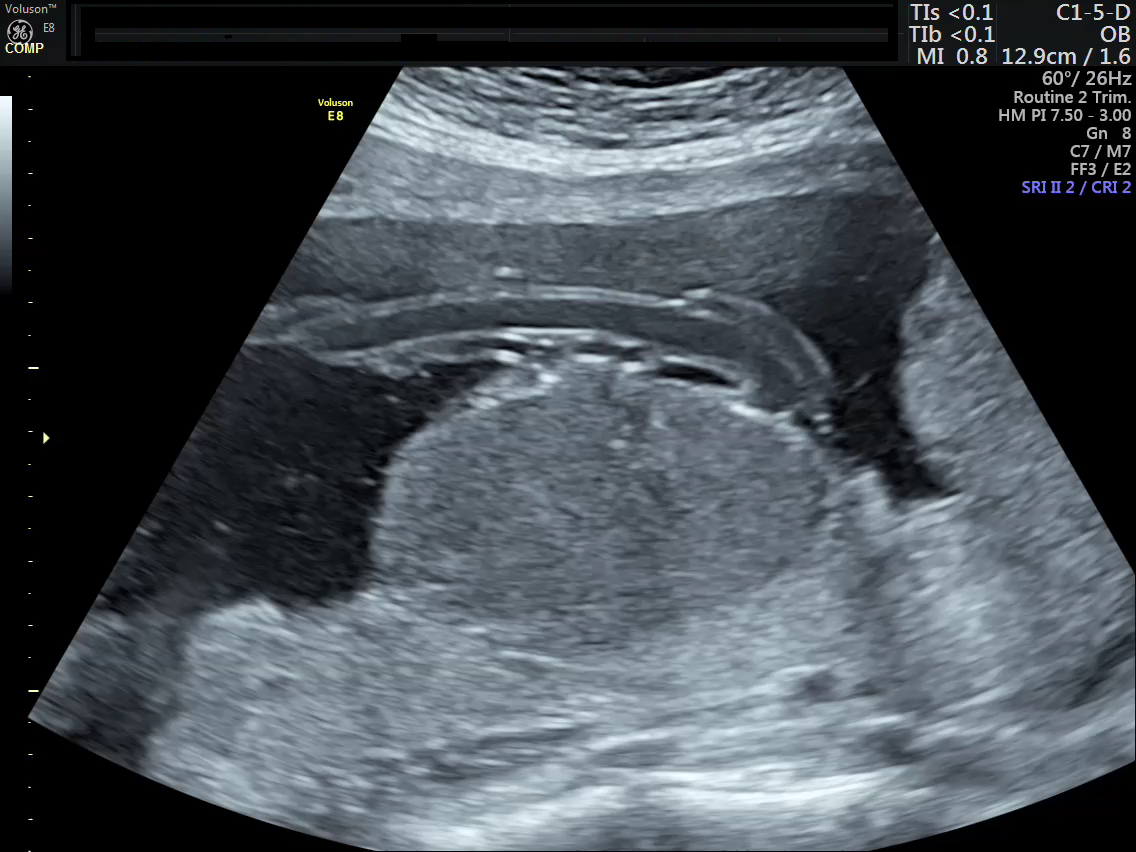
- Placenta was fundal and posterior with normal retroplacental complex.
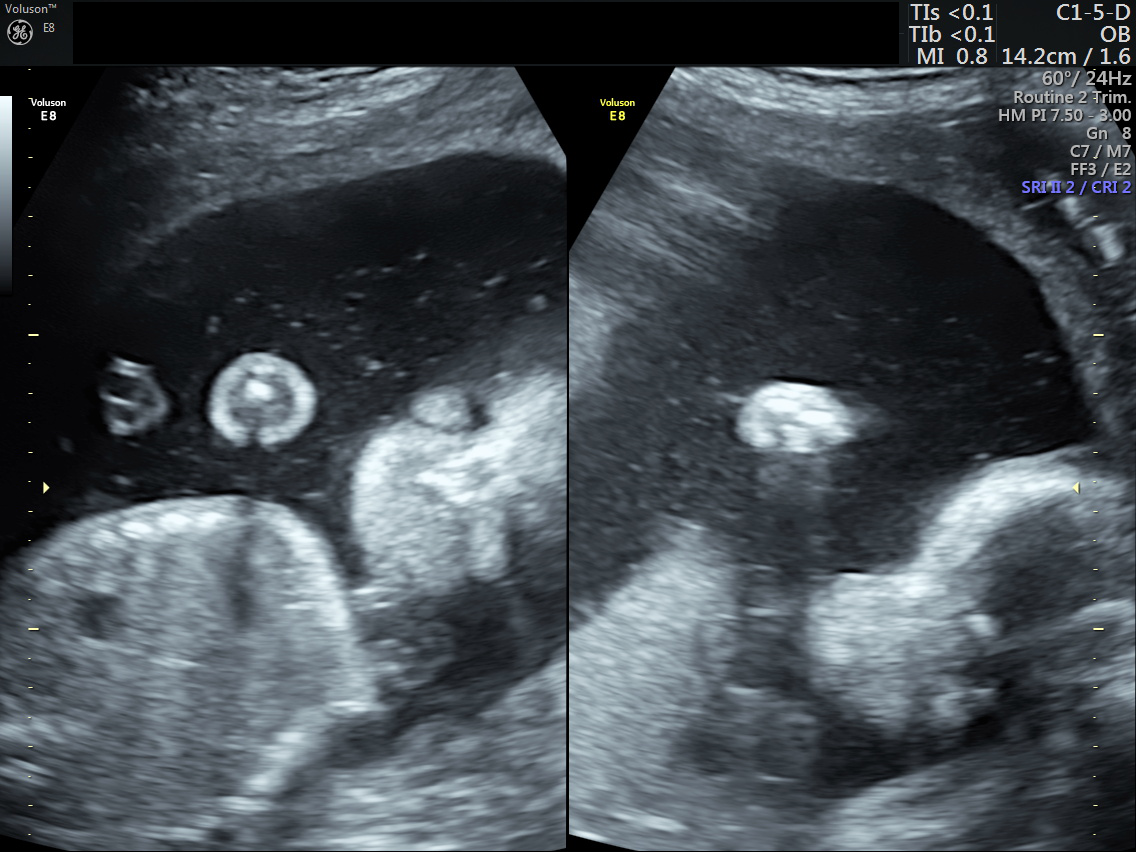
- There was a well defined, sharply marginated hypoechoic area which was identified in the sub-chorionic region of the placenta, presenting as a bulge on the fetal surface measuring 5.4 x 5.7 cms.
- The mass had uniformly homogenous echotexture.
- It was located near the insertion of the umbilical cord.
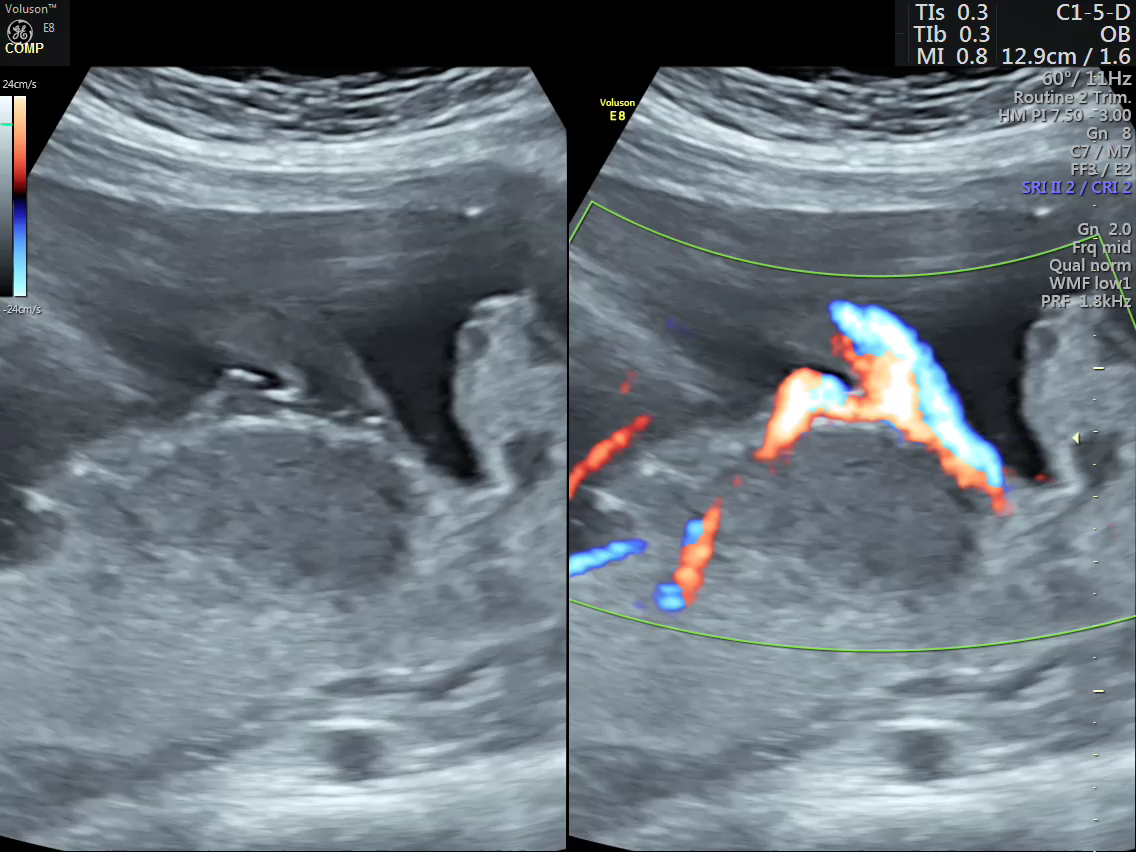
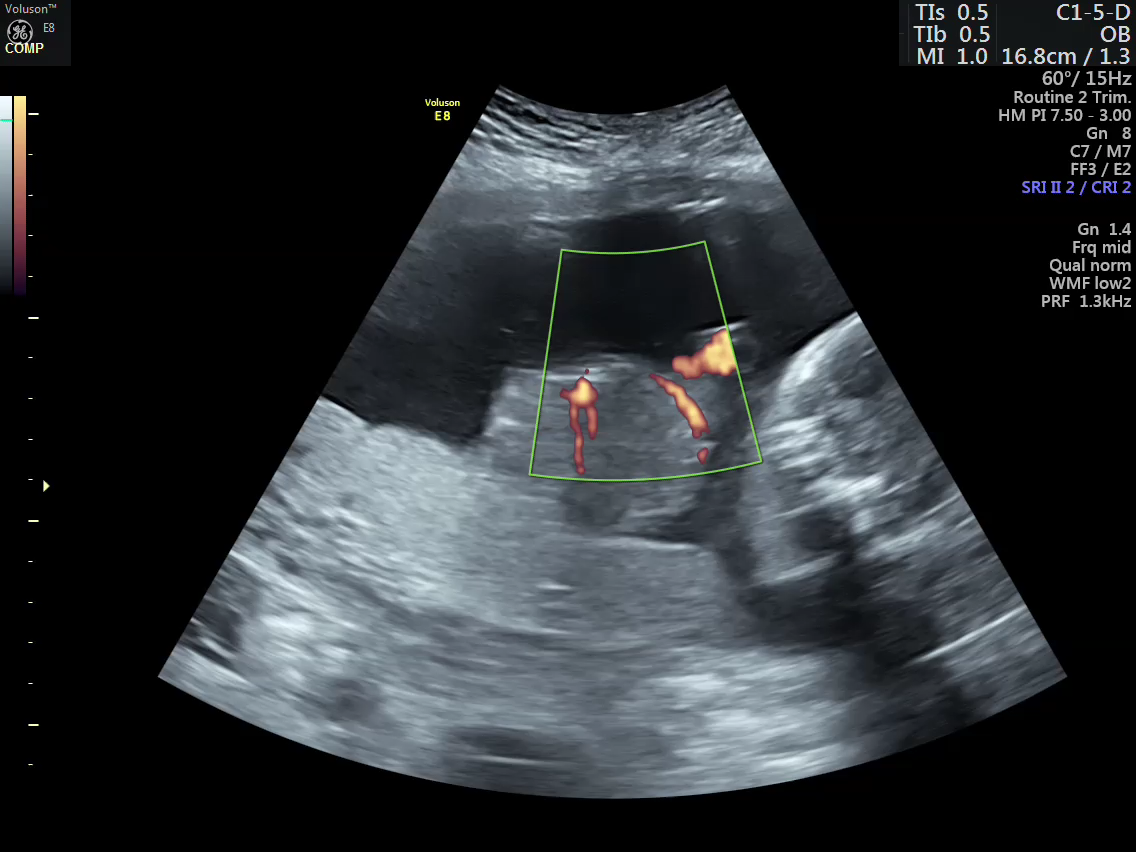
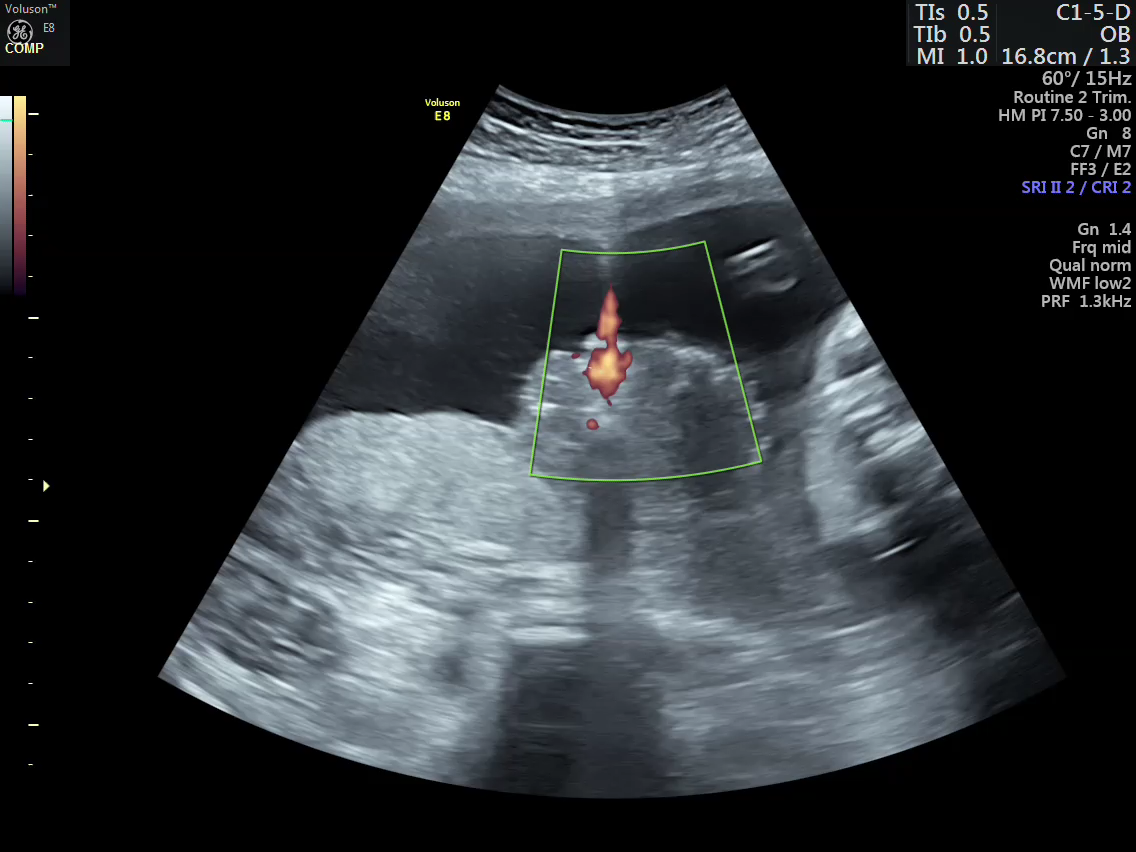
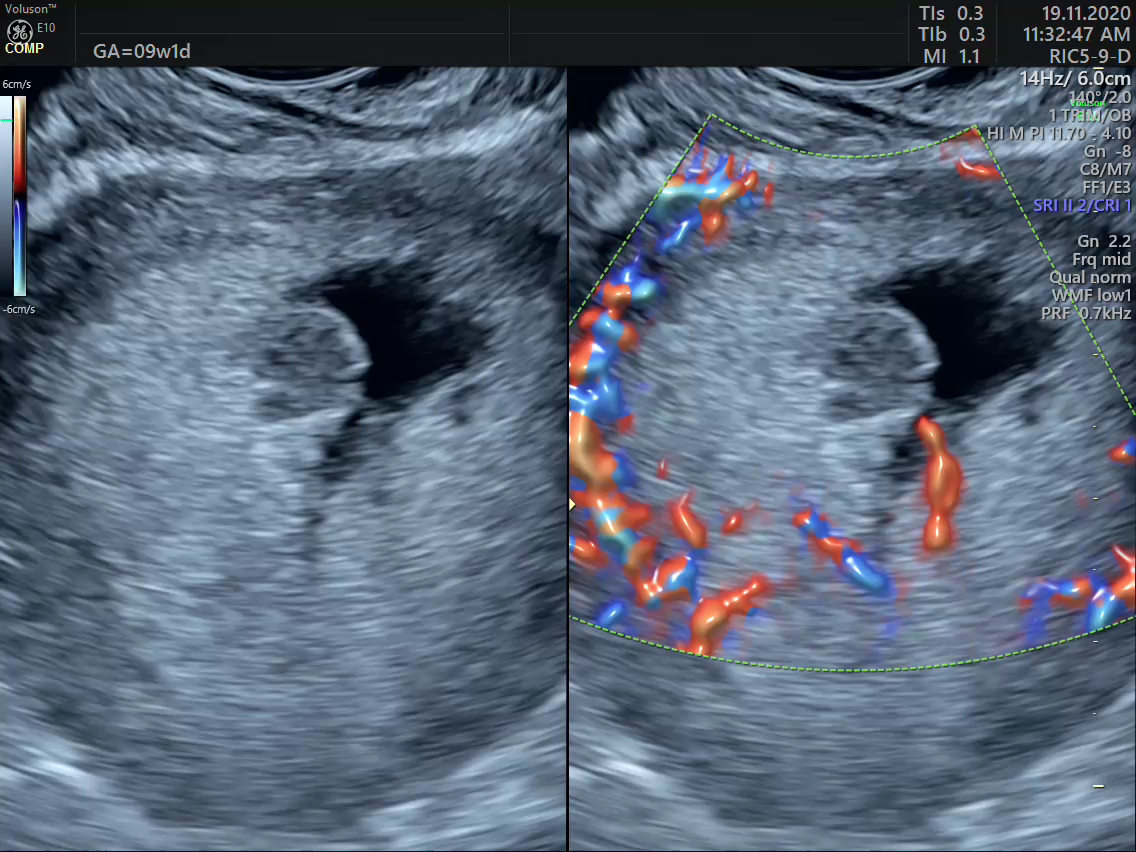
Color Doppler

Discussion
- Large chorioangiomas may result in fetal anemia and thrombocytopenia due to sequestration of red blood cells and platelets by the tumor.
- Hyperdynamic circulation due to arteriovenous shunts in the tumor can lead to fetal heart failure (pericardial effusion), hydrops and placentomegaly..
- There will be associated polyhydramnios due to direct transudation into amniotic fluid and due to fetal polyuria secondary to hyperdynamic circulation.
- These tumors can also result in maternal fluid overload and preeclampsia
Minimal pericardial effusion / polyhydramnios
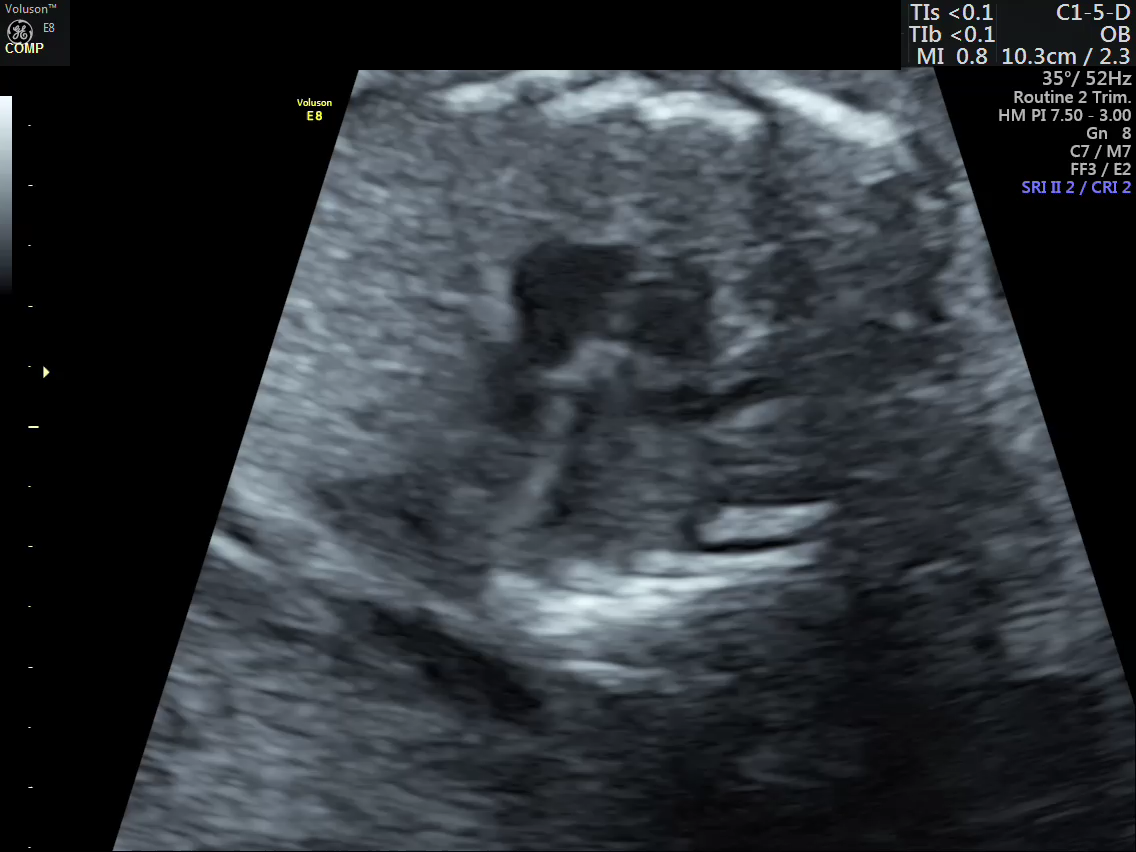
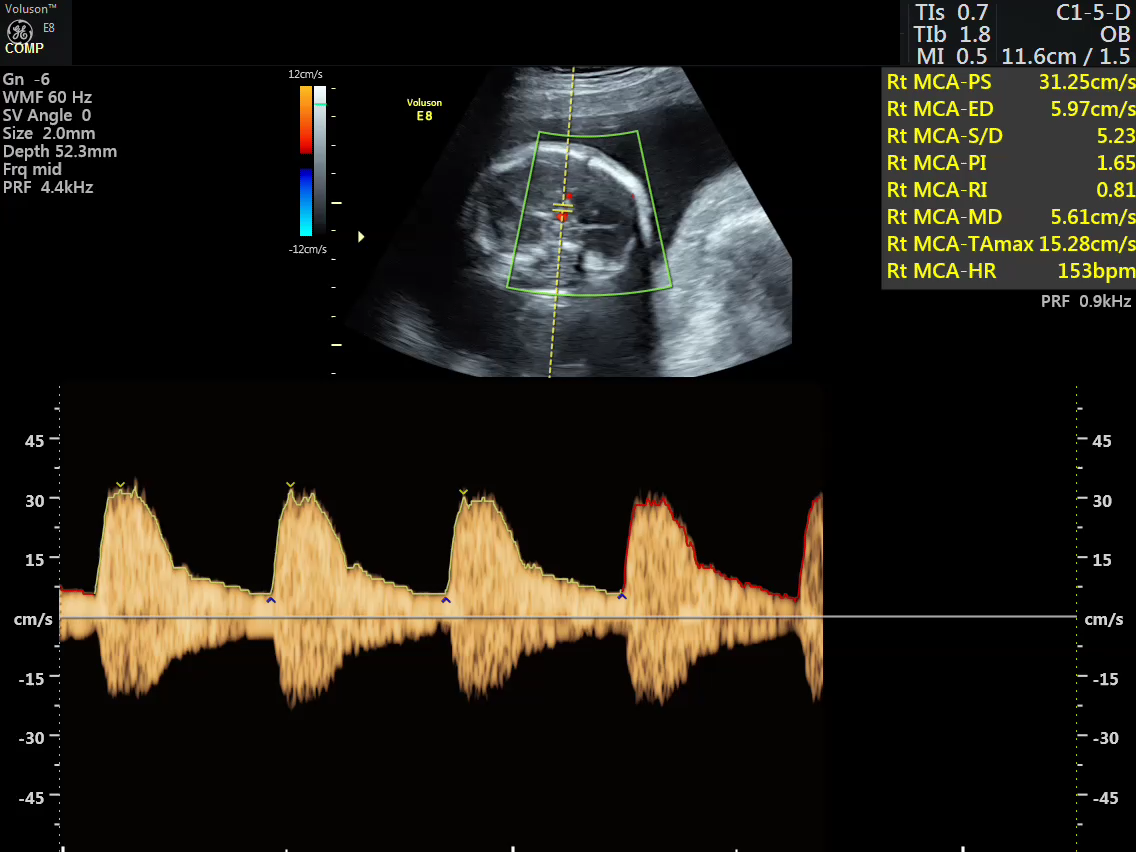
Middle Cerebral Artery Doppler
Management strategies
Management depends upon the gestational age and fetal symptoms.
Interventions are mainly aimed at blocking the vascular supply of the tumor.
Various management options - either fetoscopic or ultrasound guided procedures are available
Fetoscopic ligation Interstitial laser coagulation.
Radio frequency ablation Micro coil embolization
Intra-tumoral absolute alcohol injection Tissue glue tumor embolization
Management plan of the present case
- Management options were - expected management with regular follow up at two weekly interval.
- Planning to intervene depends on increase in size of the tumor, further increase in hydramnios or development of features of hydrops such as pericardial effusion, cardiomegaly and development of pleural/ peritoneal fluid.
- Middle cerebral artery Doppler showing increased peak systolic velocity indicating development of fetal anemia.
- In our case - The tumor was of large size, there was increased amniotic fluid and minimal pericardial effusion.
- The literature reveals ideal time to intervene is at 22 to 24 weeks with early features of fetal complications
Management adopted
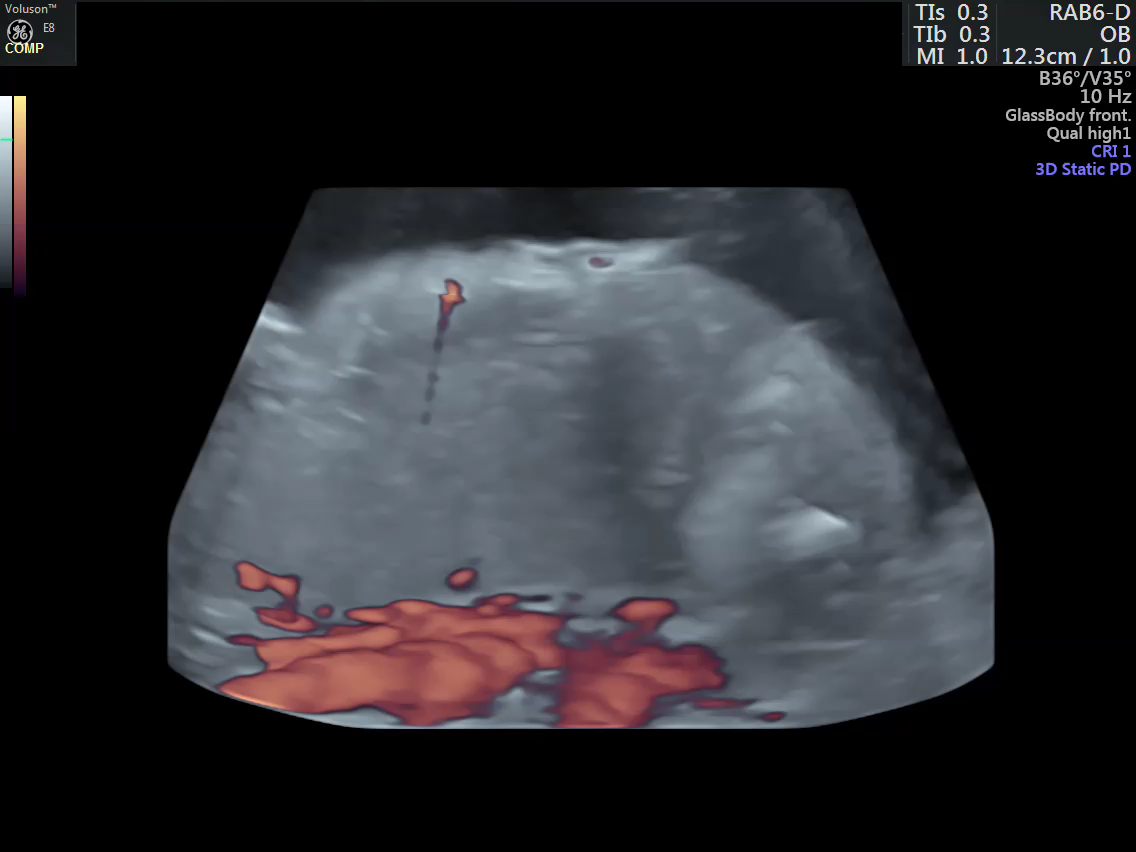
- Vascular mapping of the tumor done by 3D power Doppler angio.
- Intra-tumoral vessels identified

Ultrasound guided intra tumoral tissue glue injection
- Tissue glue- n-Butyl-2- Cyanoacrylate
- It is a liquid adhesive that polymerizes immediately upon contact with blood or body fluid.
- It has been used as an effective embolising agent in surgical conditions (e.g., cerebral arteriovenous malformations) .
- It is extensively used in interventional Radiological procedures

Procedure
|
 |
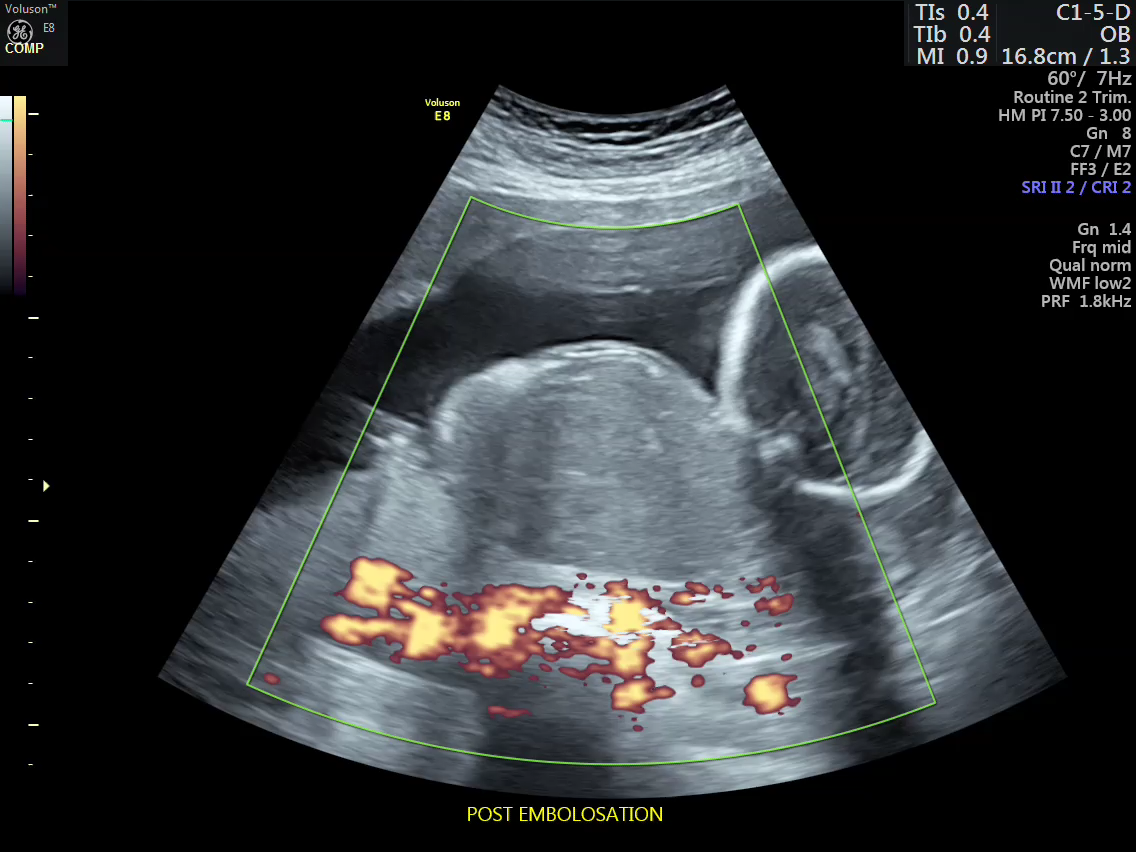
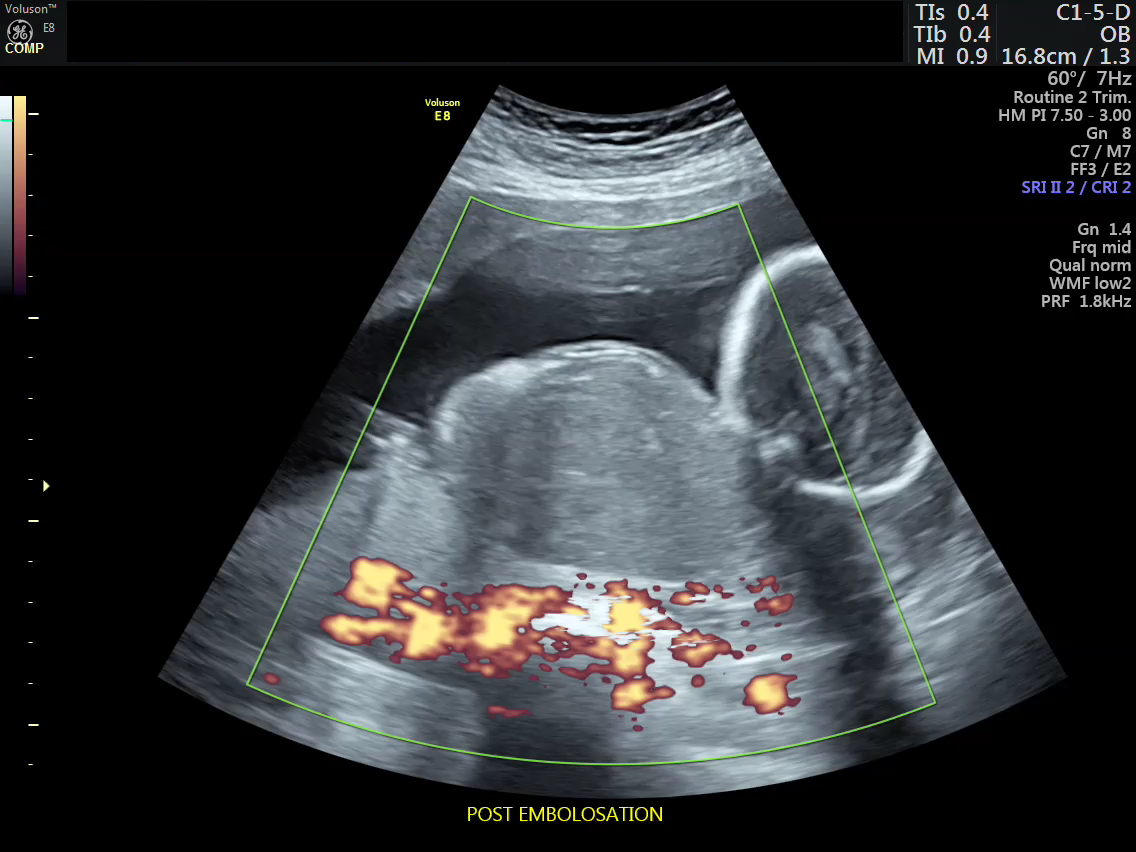
Post embolization

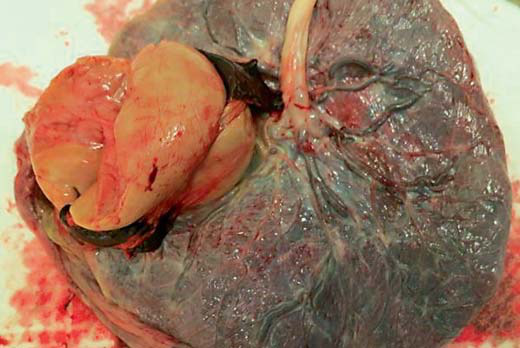
Placenta after delivery
Pale infarcted, necrosed Chorioangioma
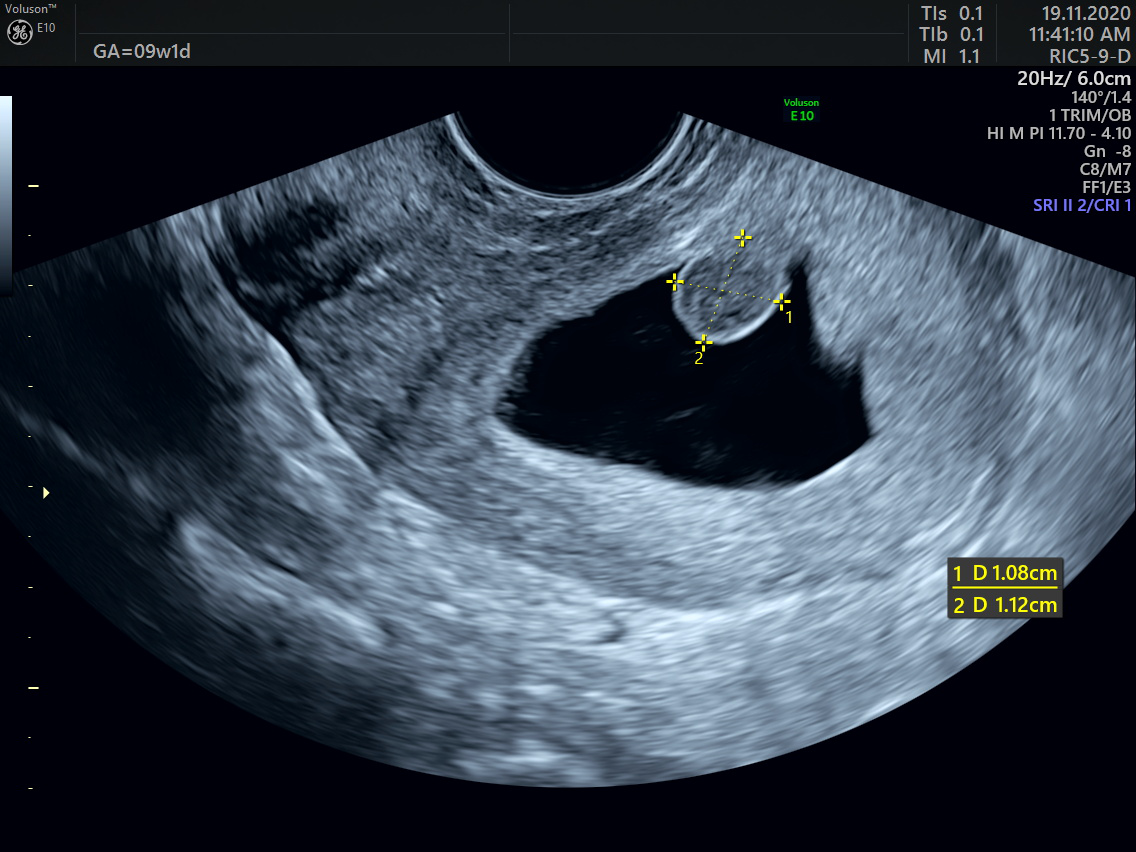
Early detection of Chorioangioma

Key learning factors
- The incidence of placental chorioangioma is 1 in 5000 pregnancies
- Size of the tumor varies.
- Small tumors are usually not detected and are asymptomatic.
- Tumors less than 5 cms can be managed expectantly resulting in spontaneous regression.
- Tumors which are large and causing fetal complications such as fetal anemia, polyhydramnios, cardiac overload and hydrops should be prenatally managed.
- Various management options are available
- Tissue glue embolization is a less invasive procedure and can be performed under local anesthesia with insignificant complications.
- Percutaneous cyanoacrylate embolization should be considered as the primary in utero therapy for placental chorioangioma.
